3 Key Steps To Improve Medical Billing Process Avoid Claim Denialsо
Tips For An Effective Medical Claims Billing Process Shawano Leader 3. create an appeals protocol for denied claims. creating a systematic approach for handling insurance claim denial is key to effective claims denial management. here are the essential steps to set up an efficient appeals protocol: review the denial: start by thoroughly reviewing the denial notice to understand why the claim was denied. this. Implementing key strategies to improve the medical billing process can have a significant impact on revenue cycle optimization and efficient claims management in healthcare organizations. by ensuring accurate patient data collection and improving the first pass yield, organizations can reduce the number of denied claims and minimize coding errors.

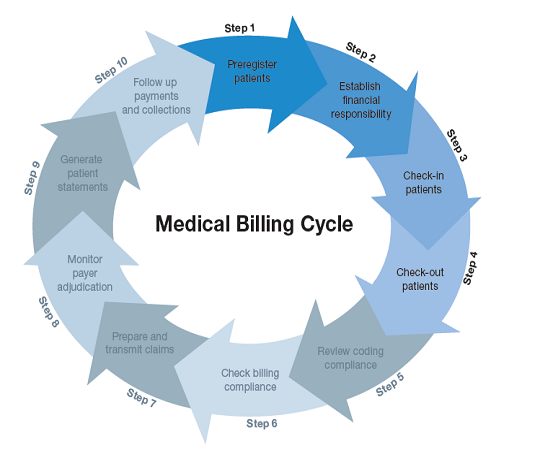
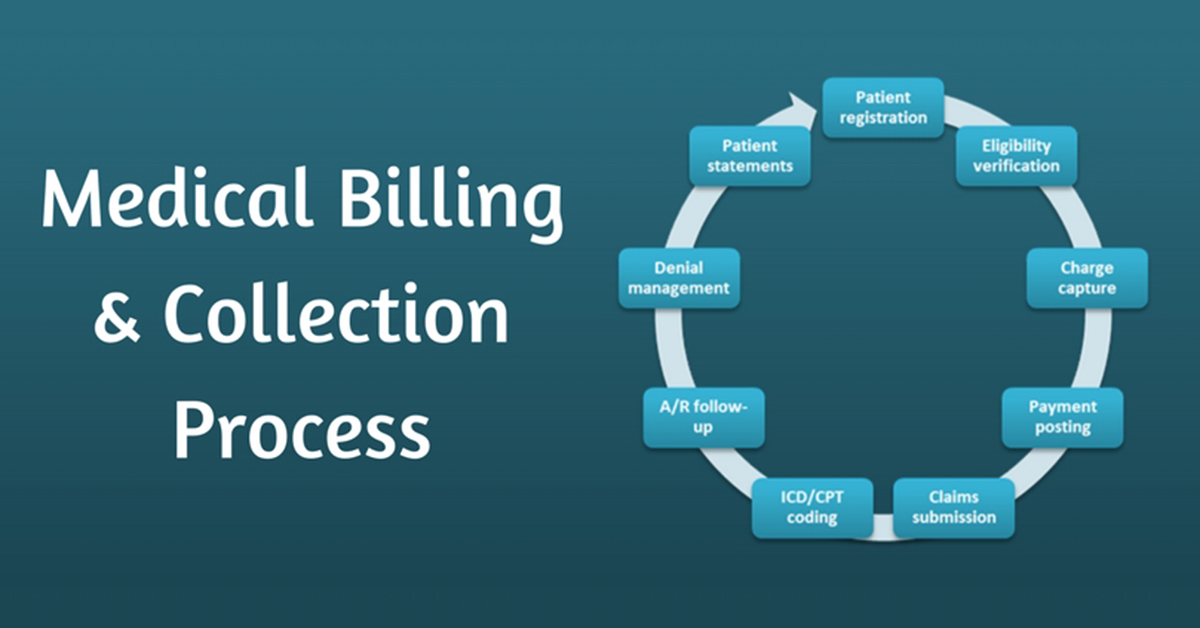
3 Key Steps To Improve Medical Billing Process Avoid Step 4: generate and transmit claims. after generating a superbill, you need to create a paper or an electronic medical claim. don’t forget to check for coding and formatting errors to avoid denials. each claim should contain the patient’s details and procedures data (cpt or hcpcs codes). Avoiding coordination of benefits denials means faster payments, better cash flow, and happier patients. bottom line: taking the time to verify means smoother billing for everyone. 2). utilize technology and ehr software. for a medical practice, claim denials due to coordination of benefits issues can be a real hassle. While the medical billing process appears overly complicated, it is a set of easy steps that, when followed with precision, make medical billing easier. these steps include: 1. demographic entries and verification. the most crucial step is to retrieve patient information; these details include the name, residence, gender, and contact. Automated software can make this step more efficient. 7. claim submission. once scrubbed, the claim is submitted to the insurance company either electronically — which is faster and more efficient — or through paper claims. 8. follow up and reconciliation. after submission, it is essential to track the claim status and follow up with the.

All You Need To Know About The Medical Billing Process While the medical billing process appears overly complicated, it is a set of easy steps that, when followed with precision, make medical billing easier. these steps include: 1. demographic entries and verification. the most crucial step is to retrieve patient information; these details include the name, residence, gender, and contact. Automated software can make this step more efficient. 7. claim submission. once scrubbed, the claim is submitted to the insurance company either electronically — which is faster and more efficient — or through paper claims. 8. follow up and reconciliation. after submission, it is essential to track the claim status and follow up with the. Medical claim denials and rejections are perhaps the most significant challenge for a physician’s practice. they have a negative impact on practice revenue and the billing department’s efficiency. educating your billers and collecting and analyzing claim data can determine trends in denials and rejections. using up to date software or a 3. A denial management system can streamline the billing process by automating claim tracking, identifying denial trends, providing real time analytics, generating appeals, and facilitating communication with payers. this helps healthcare providers address denial issues efficiently and maximize revenue. published by medical billers and coders.
What Is Medical Billing And How To Perform It Successfully Medical claim denials and rejections are perhaps the most significant challenge for a physician’s practice. they have a negative impact on practice revenue and the billing department’s efficiency. educating your billers and collecting and analyzing claim data can determine trends in denials and rejections. using up to date software or a 3. A denial management system can streamline the billing process by automating claim tracking, identifying denial trends, providing real time analytics, generating appeals, and facilitating communication with payers. this helps healthcare providers address denial issues efficiently and maximize revenue. published by medical billers and coders.
Comments are closed.